The Promises and the Dangers of AI in Mental Health
Artificial intelligence is reshaping many professions, including mental health care. Some tools offer convenience: automated note-taking, mood-tracking apps, or chatbots that promise “therapy anytime.” According to a recent HAI report from Stanford, however, these tools are far from ready to replace human therapists, and many pose real dangers to vulnerable populations.
In fact, the study found that many popular AI-powered mental-health chatbots:
-
show bias against people with substance-use disorders and severe disorders, including reluctance to “work closely with” individuals labeled with alcohol dependence or schizophrenia.
-
sometimes respond inappropriately to suicidal thoughts or crisis disclosures, failing to offer real containment or intervention.
-
reinforce stigma and may even worsen outcomes for already vulnerable people.
For vulnerable people healing from trauma, addiction, or attachment wounds, substituting a therapist with a chatbot can be not just insufficient, but potentially harmful.
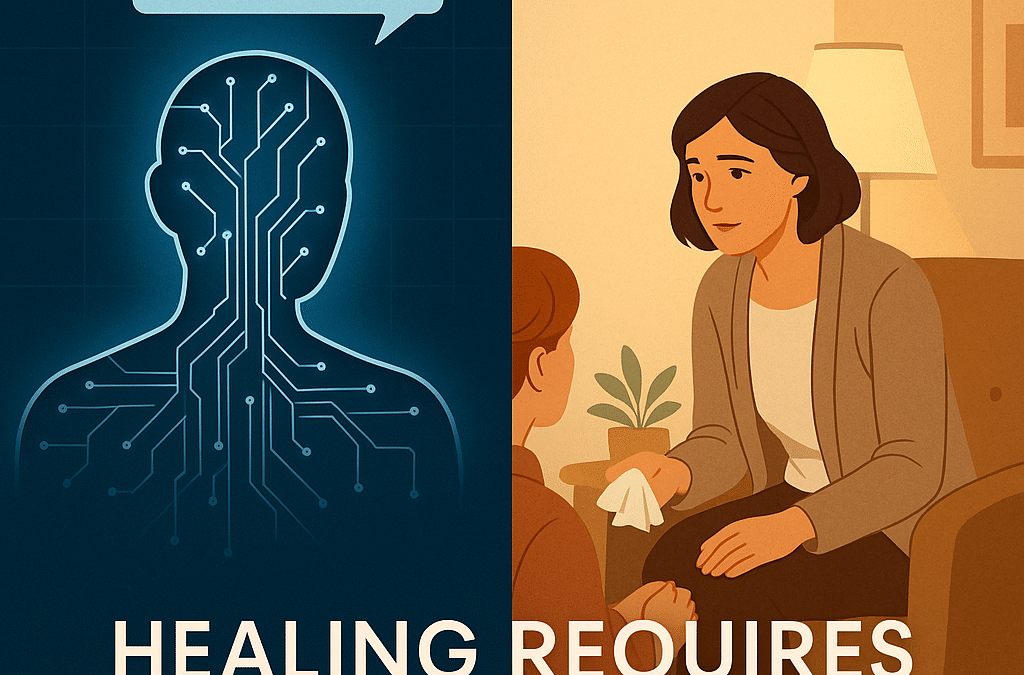
Healing Requires More Than Words. It Needs Safety, Attunement, and Human Presence
Healing is rarely a formulaic process. Especially for people with complex trauma, addiction, or long histories of neglect or unstable caregiving, the foundation of healing isn’t just talk. It’s safety, attunement, trust, and human connection. Emotional attunement is the ability to notice, understand, and respond to another person’s internal emotional state in a way that feels accurate, supportive, and connecting. When someone is emotionally attuned, they can sense what you’re feeling, stay present with you, adjust their own response to help you feel safe, and repair quickly if they misread you.
What many trauma-informed therapists describe as “misattunement” arises when early caregivers were unpredictable, emotionally unavailable, or inconsistently responsive. Over time, the nervous system learns survival strategies: hyper-vigilance, hiding emotions, people-pleasing, guarding closeness, expecting criticism or abandonment.
As a result of chronic misattunement, the body learns: “no one is coming; I must protect myself.”
Before even beginning trauma work such as EMDR, clients often need a period of safety-building and relational re-learning. For survivors of childhood emotional neglect, domestic violence, narcissistic abuse, or unpredictable caregiving, reconnecting with a consistently attuned, present therapist can feel unfamiliar, even scary.
Therapy geared toward nervous-system regulation, especially combining EMDR with body-based tools, can create a new experience of safety, emotional presence, and stable attunement.
EMDR + Safe and Sound Protocol (SSP) — A Body-Centered, Relational Path Toward Healing
When therapy combines evidence-based trauma work (EMDR) with nervous-system regulation (SSP), something shifts: healing moves beyond cognition and memory and into safety, embodiment, and new rhythms of regulation.
This approach recognizes that trauma and addiction rarely start in a single moment. They unfold over time, often rooted in early attachment wounding, neglect, misattunement, and repeated experiences of danger or abandonment.
In this work:
-
the nervous system learns new patterns of safety through consistent, attuned relationship and somatic regulation
-
the mind can begin to process and integrate traumatic memories without overwhelming the system
-
the brain’s natural healing process, the adaptive information processing (AIP) system, comes back online
That kind of healing demands a human therapist, not a chatbot.
A Vision for Ethical, Human-Centered Mental Health Care in the Age of AI
This isn’t a dismissal of technology. Thoughtfully designed AI tools can support care, with limits. Documentation support, scheduling automation, psychoeducation, and mood tracking can help reduce administrative burden and increase access.
But when it comes to healing trauma, addiction, attachment wounds, the human presence, connected attuned relationship, nervous system awareness, and clinical judgment remain non-negotiable.
At Potomac Behavioral Health, this is the commitment: to hold space, to attune, to support not just healing of the mind, but regulation of the nervous system, healing of body and self, reclaiming of safety.
If you’re seeking healing in body, mind, and nervous system, especially after trauma, addiction, or attachment wounds, what you deserve is real human care: informed, ethical, relational, body-centered. That care cannot happen through a screen alone.